Antibiotics help us to treat bacterial infections and save millions of lives each year. But they can also harm the helpful microbes residing in our gut, weakening one of our body’s first lines of defence against pathogens and compromising the multiple beneficial effects our microbiota has for our health. Common side effects of this collateral damage of antibiotics are gastrointestinal problems and recurrent Clostridioides difficile infections. They also include long-term health problems, such as the development of allergic, metabolic, immunological or inflammatory diseases.
Researchers from the Typas group at EMBL Heidelberg, the Maier lab at the Cluster of Excellence ‘Controlling Microbes to Fight Infections’ at the University of Tübingen, and collaborators have analysed the effects of 144 antibiotics on our most common gut microbes. The study published in the journal Nature substantially improves our understanding of antibiotics’ effects on gut microbes. It also suggests a new approach to mitigating the adverse effects of antibiotics therapy on the gut microbiome.
The human gut harbours an intricate community of different microbial species as well as many viruses, collectively referred to as the gut microbiome. Together, they enable us to use nutrients more efficiently and hinder pathogenic bacteria from settling in our gut. However, when we treat a bacterial infection with antibiotics, there’s a risk of damaging the gut microbiome.
“Many antibiotics inhibit the growth of various pathogenic bacteria. This broad activity spectrum is useful when treating infections, but it increases the risk that the microbes in our gut are targeted as well,” explained Lisa Maier, DFG Emmy Noether group leader at the University of Tübingen. Maier is an alumna of the Typas lab and one of the two lead authors of the study.
If certain gut bacteria are harmed more than others, antibiotics therapy can lead to an imbalance in our microbiota composition, commonly referred to as dysbiosis. Diarrhoea is a common short-term effect, while allergic conditions such as asthma or food allergies and obesity are possible long-term consequences. The fact that antibiotics are also active against gut microbes has been known for a long time, but their effects on the large diversity of microbes we carry in our gut had not yet been studied systematically, mostly due to technical challenges.
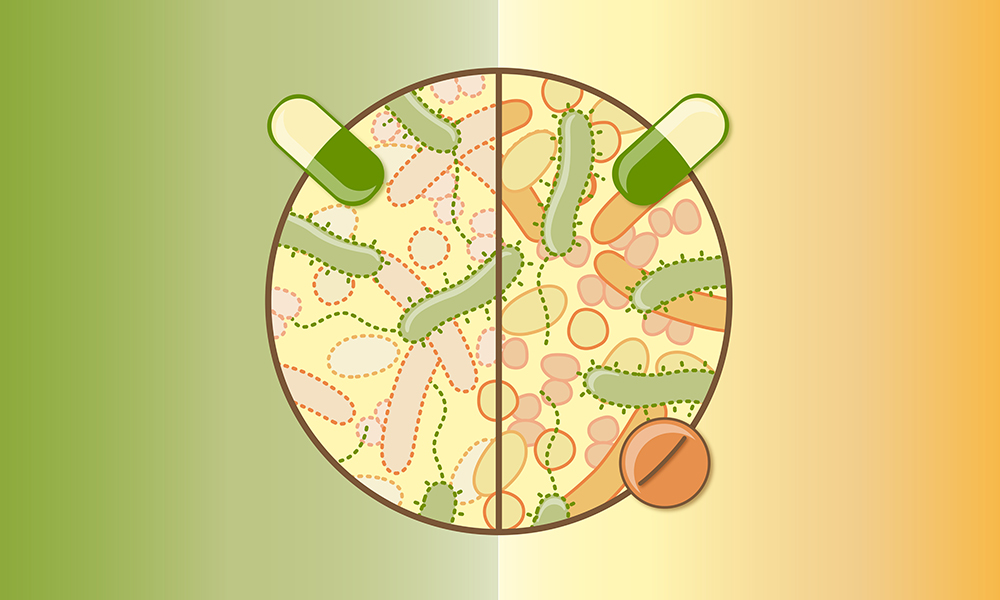
Antibiotics help our body to get rid of bacterial infections. But they can also harm the helpful microbes in our gut. EMBL scientists studied the collateral damage antibiotics cause and found that some drugs could protect many gut bacteria from antibiotics. Credit: Isabel Romero Calvo/EMBL
“So far, our knowledge of the effects of different antibiotics on individual members of our gut microbial communities has been patchy. Our study fills major gaps in our understanding of which type of antibiotic affects which types of bacteria, and in what way,” said Nassos Typas, Senior Scientist and Group Leader at EMBL Heidelberg.
Building on a previous study from EMBL’s Typas, Bork, Patil, and Zeller groups, the scientists observed how each of the 144 antibiotics affected the growth and survival of up to 27 bacterial strains commonly inhabiting our guts. The researchers determined the concentrations at which a given antibiotic would affect these bacterial strains for more than 800 antibiotic–strain combinations, expanding existing datasets on antibiotic spectra in gut bacterial species by 75%.
Importantly, the experiments revealed that tetracyclines and macrolides – two commonly used antibiotics families – not only stopped bacteria from growing, but also lead to their death. About half of the tested gut strains did not survive treatment with these types of antibiotics.
“We didn’t expect to see this effect with tetracyclines and macrolides, as these antibiotic classes were considered to have only bacteriostatic effects – which means that they stop bacterial growth, but don’t kill bacteria,” said Camille Goemans, a postdoctoral fellow in the Typas group who shares first authorship with Maier. “Our experiments show that this assumption is not true for about half of the gut microbes we studied. Doxycycline, erythromycin, and azithromycin, three commonly used antibiotics, killed several abundant gut microbial species, whereas others they just inhibited.”
The selective killing of specific microbes by tetracyclines and macrolides could lead to these microbes being inadvertently lost from the gut microbiota much faster than microbes for which growth is only inhibited, as the authors showed with synthetic microbial communities. This could explain the strong microbiota shifts that some patients being treated with these antibiotics witness.
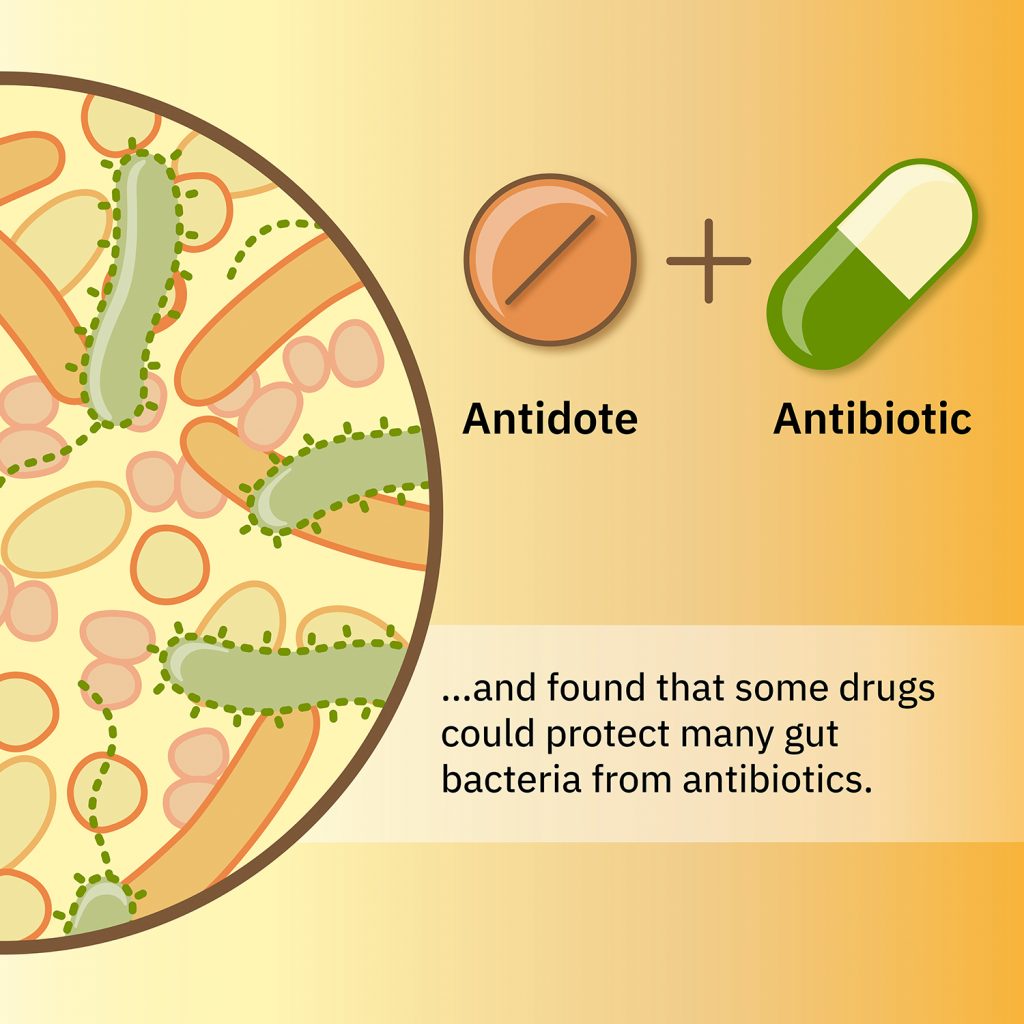
There is a way of reducing the damage, though. “We have shown before that drugs interact differently across different bacterial species. We therefore explored whether a second drug could mask the harmful effects of antibiotics on abundant gut microbes, but allow antibiotics to retain their activity against pathogens. This would provide something like an antidote, which would reduce the collateral damage of antibiotics on gut bacteria,” explained Typas.
The scientists combined the antibiotics erythromycin or doxycycline with a set of nearly 1,200 pharmaceuticals, to identify drugs that would save two abundant gut bacterial species from the antibiotic. Indeed, the researchers identified several non-antibiotic drugs that could rescue these gut microbes and other related species. Importantly, the combination of an antibiotic with a protective second drug did not compromise the antibiotics’ efficacy against pathogenic bacteria.
Follow-up experiments indicated that this approach may be working in the context of a natural microbiome as well. With help from collaborators, the scientists showed that the combination of erythromycin with an antidote mitigated the loss of certain abundant gut bacterial species from the mouse gut. Similarly, antidote drugs protected human gut microbes from erythromycin in complex bacterial communities derived from stool samples.
“Our approach that combines antibiotics with a protective antidote could open new opportunities for reducing the harmful side effects of antibiotics on our gut microbiomes,” concluded Maier. “No single antidote will be able to protect all the bacteria in our gut – especially since those differ so much across individuals. But this concept opens up the door for developing new personalised strategies to keep our gut microbes healthy.”
Further research will be needed to identify the optimal combinations, dosing, and formulations for antidotes, and to exclude potential long-term effects on the gut microbiome. In the future, the new approach may help to keep our gut microbiome healthy and reduce antibiotics’ side effects in patients, without compromising the efficiency of our antibiotics as lifesavers.
The study was a collaborative effort, involving researchers from EMBL’s Typas, Bork, Zeller, Zimmermann, and Patil groups, as well as colleagues at the University of Tübingen, Ludwig-Maximilians-Universität München, and the Max Delbrück Center for Molecular Medicine in Berlin.
Marius Bruer


