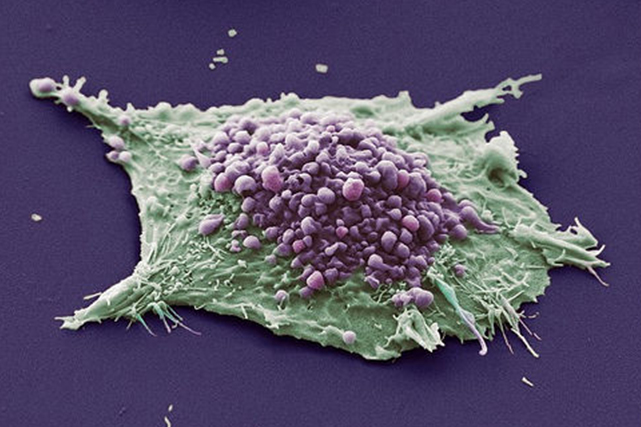
Lung cancer cell
Mutations in the p53 gene are found in more than half of all cancers, but it remains difficult to effectively target the gene with drugs even decades after its discovery. Though previous research has shown that p53 acts as a tumor suppressor and initiates cancer cell death in its natural state, a new study led by Sumitra Deb, Ph.D., suggests that gain-of-function (GOF) mutations — a type of mutation where the changed gene has an added function — turn p53 into an oncogene, causing cells to replicate uncontrollably and contribute to cancer development.
Recently published in Nature Communications, the researchers determined that mutant p53 genes are empowered by a specific protein, PLK3, to copy their genetic code and promote tumor cell proliferation through a process called transactivation.
Using preclinical models of lung cancer driven by p53 GOF mutations, Deb and his research team discovered that PLK3 activates an amino acid called serine 20 (S20), a cellular building block they found to play an important role in cancer cell replication.
By inhibiting PLK3 in GOF p53 mutant cells, they observed a decrease in the function of S20 along with overall reductions in transactivation and tumor cell formation.
“Our research indicates that GOF p53 exploits PLK3 to trigger its transactivation capability and exert oncogenic functions, raising the possibility of targeting p53-driven cancer cells using PLK3 inhibitors,” said Deb, a member of the Cancer Biology research program at Massey and professor in the Department of Biochemistry and Molecular Biology at the VCU School of Medicine.
Deb’s team will continue to explore the potential for PLK3 inhibitors to be effective drugs in the treatment of lung cancer and potentially other forms of disease with the same genetic mutation.
Sumitra Deb collaborated on this research with Brad Windle, Ph.D., Jolene Windle, Ph.D., Raghavendra Pillappa, M.D., and Swati Deb, M.S., Ph.D., members of the Cancer Biology research program at VCU Massey Cancer Center; Catherine Vaughan, Ph.D., Shilpa Singh and Mark Subler, Ph.D., of the VCU School of Medicine; Steven Grossman, M.D., Ph.D., physician-in-chief at USC Norris Comprehensive Cancer Center and former deputy director at Massey; Andrew Yeudall, Ph.D., of Georgia Cancer Center at Augusta University; and Elizabeth Fry and Kazushi Inoue, M.D., Ph.D., of the Wake Forest University School of Medicine.
This research was supported by the National Institutes of Health (CA106314, CA107532, CA121144, CA17266, CA212967, CA238515, DE024381), Pilot Project Awards from VCU Massey Cancer Center, the Jeffress Trust Foundation and, in part, with funding from Massey’s Cancer Center Support Grant (CA016059).
Written by: Blake Belden
masseycancercenter.org


