Nothing predicts the risk of heart disease more than age. Although seen at any age, rates of heart disease increase markedly in older people. It remains not only the leading cause of death in our community, but also the key reason many older people cannot perform the physical activities they want and need for daily life.
Given our increasing lifespan, we need to better understand how and why the heart and blood vessels (cardiovascular system) age, and whether we can slow down the processes involved.
Heart disease can cause heart attack, angina, heart failure or eventually, sudden cardiac death. Heart disease includes stroke, aneurysm and other diseases of the arteries — the tubes that carry oxygenated blood from the heart to parts of the body.
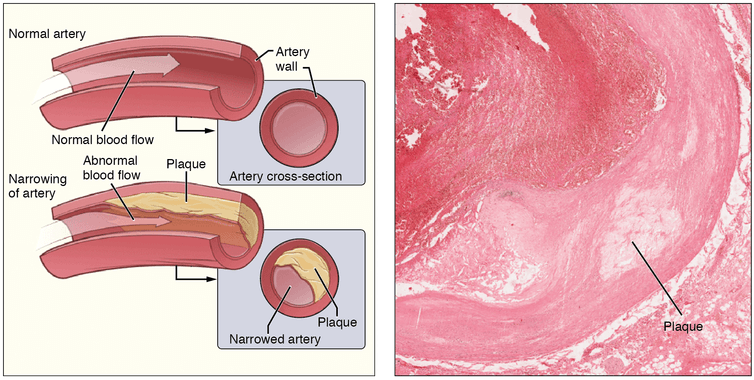
Most of this list of serious conditions can be traced back to atherosclerosis in our arteries. This refers to build up of cholesterol and other factors such as modified cholesterol, cellular debris and cells associated with inflammation in the walls of arteries that obstructs blood flow. This leads to a blockage due to blood clots (thrombosis).
What happens in the heart as we age?
Does the heart wear out? Is there a timer ticking away somewhere in our body that eventually says «enough," or do we cumulatively inflict damage over time?
The simple answer is: a little bit of the first two and quite a lot of the third. Continuous exposure to the risk factors for heart disease over decades plays a large part. Tobacco products, high blood pressure, abnormal blood fats and diabetes are all
Ageing particularly affects the structure and function of arteries. Two important structural protein fibres hold the larger arteries together: collagen and elastin.
Collagen is inelastic but strong. It takes most of the burden of the pressure inside arteries brought about by the power of the heart pumping blood around the body.
As the name suggests, elastin is elastic, and has many of the characteristics of rubber. By stretching when the heart pumps blood, elastin helps cushion the fluctuations in pressure inside the artery. Like rubber, it is extremely tolerant of repetitive stretching and relaxation. But like rubber, it will eventually wear out.
After decades of repetitions (60 to 80 times a minute, 24 hours a day) more of the load is taken by the stiffer collagen and less by the softer, compliant elastin. As there is now less cushioning of each powerful beat of the heart, the systolic blood pressure (the peak pressure when the heart is actively pumping blood into the arteries) increases.
Blood moves more quickly through stiffer pipes so the diastolic blood pressure (the lowest pressure with each beat when the heart is relaxing and refilling) tends to fall.
Older people with stiff arteries have a bigger difference between their systolic and diastolic blood pressures. Regular physical activity, healthy nutrition and a good hormonal balance can delay this process.
What are the effects of the ageing heart?
High systolic pressure damages the walls of arteries. There are also other consequences downstream in the very small arteries that feed oxygen and nutrients to the organs of the body. They are subjected to a faster moving pulse of blood at a higher pressure, which rapidly falls away.
This means they’re pulled and stretched more vigorously with each beat, and that disturbs their function. Damage to small arteries in the brain can cause multiple tiny strokes, the cause of many cases of dementia.
Damage to arteries in the kidney results in impaired function. As the kidney has an important role in regulating blood pressure in the rest of the body, a vicious cycle can be established where high blood pressure begets more high blood pressure, and more kidney damage leads to kidney failure.
The most vulnerable part of our arteries is the inner lining of their walls. This plays a vital function, acting as a barrier between the blood stream and the wall of the artery as well as controlling the function of the muscle layer of the wall. This widens or narrows the artery in accord with the oxygen needs of the organs of the body.
If they are damaged by tobacco smoke, a poor diet, diabetes or other risk factors, this barrier function can be lost, allowing the various ingredients of atherosclerosis to accumulate in the wall.
Atherosclerosis in the coronary arteries causes narrowing which can progress to blockage. Age is not necessarily the problem here but these build up over time and the longer the exposure to these damaging factors the more likely heart disease will emerge.
As collagen is the major structural protein in the ageing heart, it is stiffer. Heart muscle cells are not replaced as quickly as they are lost. This less elastic heart does not fill as well, may not empty as well and therefore does not pump as well.
Heart failure is when the pumping ability has fallen to the extent the blood supply to the body is insufficient to meet the needs of daily living. Fortunately this only occurs after the vast reserve capacity of the healthy heart has been overcome.
Another consequence of these changes is that the electrical impulses the heart generates to activate each beat travel less efficiently across the heart. This is a cause of atrial fibrillation, a form of irregular heart beat that can lead to stroke, especially in older people.
Ageing of our cells is a lifelong race between production of new cells and loss of the old. As we get older the loss due to
This is one of several natural processes that provide a ticking clock for our heart muscle. Staying physically and mentally active, being aware of the things that damage your arteries and having regular heart checks is the way to healthy ageing.
Source: https://theconversation.com/heart-disease-what-happens-when-the-ticker-wears-and-tears-69150


