Extended cardiac monitoring in patients and the use of implantable cardiovascular electronic devices can increase detection of atrial fibrillation (AF), but the devices have limitations including short battery life and lack of immediate feedback. Can new smartphone tools that can record an electrocardiogram (ECG) strip and make an automated diagnosis overcome these limitations and facilitate timely diagnosis? The largest study to date, in the Canadian Journal of Cardiology, published by Elsevier, finds that the use of these devices is challenging in patients with abnormal ECGs. Better algorithms and machine learning may help these tools provide more accurate diagnoses, investigators say.
“Earlier studies have validated the accuracy of the Apple Watch for the diagnosis of AF in a limited number of patients with similar clinical profiles,” explained lead investigator Marc Strik, MD, PhD, LIRYC institute, Bordeaux University Hospital, Bordeaux, France. “We tested the accuracy of the Apple Watch ECG app to detect AF in patients with a variety of coexisting ECG abnormalities.”
The study included 734 consecutive hospitalized patients. Each patient underwent a 12-lead ECG, immediately followed by a 30-second Apple Watch recording. The smartwatch’s automated single-lead ECG AF detections were classified as “no signs of atrial fibrillation,” “atrial fibrillation,” or “inconclusive reading.” Smartwatch recordings were given to an electrophysiologist who conducted a blinded interpretation, assigning each tracing a diagnosis of “AF,” “absence of AF,” or “diagnosis unclear.” A second blinded electrophysiologist interpreted 100 randomly selected traces to determine the extent to which the observers agreed.
In approximately one in every five patients, the smartwatch ECG failed to produce an automatic diagnosis. The risk of having a false positive automated AF detection was higher for patients with premature atrial and ventricular contractions (PACs/PVCs), sinus node dysfunction, and second- or third-degree atrioventricular-block. For patients in AF, the risk of having a false negative tracing (missed AF) was higher for patients with ventricular conduction abnormalities (interventricular conduction delay) or rhythms controlled by an implanted pacemaker.
The cardiac electrophysiologists had a high level of agreement for differentiation between AF and non-AF. The smartphone app correctly identified 78% of the patients who were in AF and 81% who were not in AF. The electrophysiologists identified 97% of the patients who were in AF and 89% who were not.
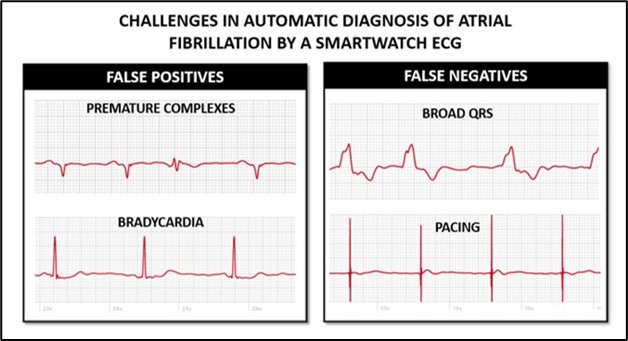
Caption: Example of false positive (failure to diagnose a normal ECG in patient without AF) electrocardiograms (ECGs) caused by occurrence of premature complexes or bradycardia and false negative (failure to detect AF in a patient with AF) ECGs caused by broad QRS complexes and ventricular pacing (Credit: Canadian Journal of Cardiology).
Patients with PVCs were three times more likely to have false positive AF diagnoses from the smartwatch ECG, and the identification of patients with atrial tachycardia (AT) and atrial flutter (AFL) was very poor.
“These observations are not surprising, as smartwatch automated detection algorithms are based solely on cycle variability,” Dr. Strik noted, explaining that PVCs cause short and long cycles, which increase cycle variability. “Ideally, an algorithm would better discriminate between PVCs and AF. Any algorithm limited to the analysis of cycle variability will have poor accuracy in detecting AT/AFL. Machine learning approaches may increase smartwatch AF detection accuracy in these patients.”
In an accompanying editorial, Andrés F. Miranda-Arboleda, MD, and Adrian Baranchuk, MD, Division of Cardiology, Kingston Health Science Center, Kingston, ON, Canada, observed that this is the first “real-world” study focusing on the use of the Apple Watch as a diagnostic tool for AF.
“It is of remarkable importance because it allowed us to learn the performance of the Apple Watch in the diagnosis of AF is significantly affected by the presence of underlying ECG abnormalities. In a certain manner, the smartwatch algorithms for the detection of AF in patients with cardiovascular conditions are not yet smart enough. But they may soon be,” Dr. Miranda-Arboleda and Dr. Baranchuk said.
“With the growing use of smartwatches in medicine, it is important to know which medical conditions and ECG abnormalities could impact and alter the detection of AF by the smartwatch in order to optimize the care of our patients,” Dr Strik said. “Smartwatch detection of AF has great potential, but it is more challenging in patients with pre-existing cardiac disease.”
Media contact: Eileen Leahy


