The adoptive T-cell therapy ADP-A2M4, which is engineered to express a T-cell receptor (TCR) directed against the MAGE-A4 cancer antigen, achieved responses in patients with multiple solid tumor types, including #102synovial sarcoma, head and neck cancer and lung cancer, according to results from a Phase I clinical trial led by researchers at The University of Texas MD Anderson Cancer Center.
Among 38 patients treated on the trial, the ADP-A2M4 T cells resulted in overall response (OR), or tumor shrinkage, in 9 patients (23.7%) and stable disease in 18 patients (47.4%). Trial data were shared in an oral presentation at the 2020 American Society of Clinical Oncology Annual Meeting by principal investigator David Hong, M.D., professor of Investigational Cancer Therapeutics.
“Thus far, we haven’t seen strong responses in treating solid tumors with available cellular therapies, in large part because antigens expressed are not restricted to the tumors,” said Hong. “In this trial, I’ve been encouraged to see durable responses in several patients, and the results suggest there is potential for this emerging TCR-based technology for treating solid tumors.”
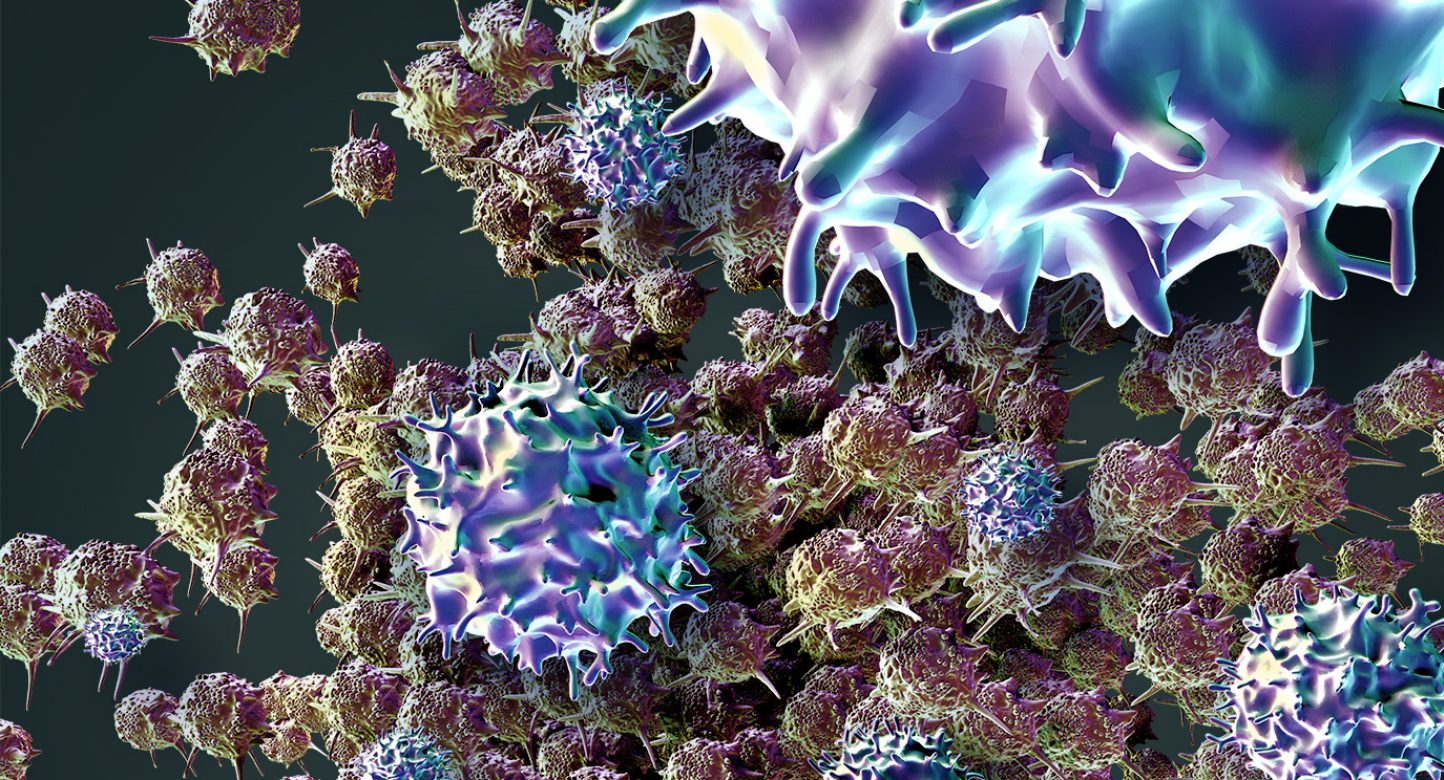
Adoptive cellular therapy is a form of immunotherapy that modifies immune cells to be more effective in mounting an immune response against cancer. For ADP-A2M4, T cells are isolated from patients and engineered to express a TCR targeting MAGE-A4, a protein normally expressed only in the testis but present in certain cancers.
Unlike chimeric antigen receptor (CAR)-modified T cells, which target surface proteins on cancer cells, TCR T-cell therapies are able to target proteins normally found inside the cell by recognizing protein fragments bound to immune-related proteins on the cell surface.
The Phase I trial was designed as a dose-escalation study to assess the safety, tolerability and antitumor activity of ADP-A2M4 in patients with advanced solid tumors with expression of the MAGE-A4 protein. Patients on the trial included those with synovial sarcoma, ovarian cancer, head and neck cancer, gastric cancer, myxoid/round cell liposarcoma, non-small cell lung cancer, bladder cancer, esophageal cancer and melanoma. Participants had a median of three prior lines of systemic therapy.
The therapy achieved strong responses in particular groups of patients in the trial. Patients with synovial sarcoma saw a 43.8% OR rate and a disease control rate of more than 90%. There also was an additional patient with an unconfirmed response after the data cut-off. Median duration of response in these patients was 28 weeks and median progression-free survival was 20 weeks. Confirmed responses were also seen in patients with lung cancer and head and neck cancer.
Most patients (97.4%) experienced some treatment-related adverse events, with the most common being low blood cell counts (lymphopenia, leukopenia, neutropenia, anemia and thrombocytopenia). Half of patients experienced cytokine release syndrome. Two patients had trial-related deaths, which led to modification of the lymphodepletion regimen and eligibility criteria.
“The side effects seen on the trial were largely consistent with those typically experienced by cancer patients undergoing lymphodepleting chemotherapy and cellular therapy,” said Hong. “This study is a nice proof of concept for treating solid tumors and suggests there could be a role for cellular therapies in these indications going forward.”
This research is part of an ongoing strategic alliance between MD Anderson and Adaptimmune, designed to expedite the development of novel T-cell therapies for multiple cancer types. Translational research and analyses of related biomarkers continues. Results from this study led to a low-dose radiation sub-study, a Phase II trial of ADP-A2M4 in sarcoma and a Phase I trial of Adaptimmune’s next-generation T-cell therapy targeting MAGE-A4, ADP-A2M4CD8.
MD Anderson
mdanderson.org


