Human organ transplants offer a crucial lifeline to people with serious illnesses, but there are too few organs to go around: in the U.S. alone, there are more than 112,000 people currently waiting for transplants. The promise of 3D printing organs is one possible solution to address this shortage but has been fraught with complexity and technical barriers, limiting the type of organs that can be printed. Researchers at Stevens Institute of Technology are now pushing through these barriers by leveraging a decades-old technique to reproduce any tissue type.
The work, led by Robert Chang, an associate professor in the mechanical engineering department at Stevens’ Schaefer School of Engineering & Science, could open up pathways for 3D printing any kind of organ at any time, even skin directly on an open wound.
“Creating new organs to order and saving lives without the need for a human donor will be an immense benefit to healthcare,” said Robert Chang, whose work appears in the April issue of Scientific Reports. “However, reaching that goal is tricky because printing organs using “bio-inks” — hydrogels laden with cultured cells — requires a degree of fine control over the geometry and size of printed microfibers that current 3D printers simply can’t achieve.”
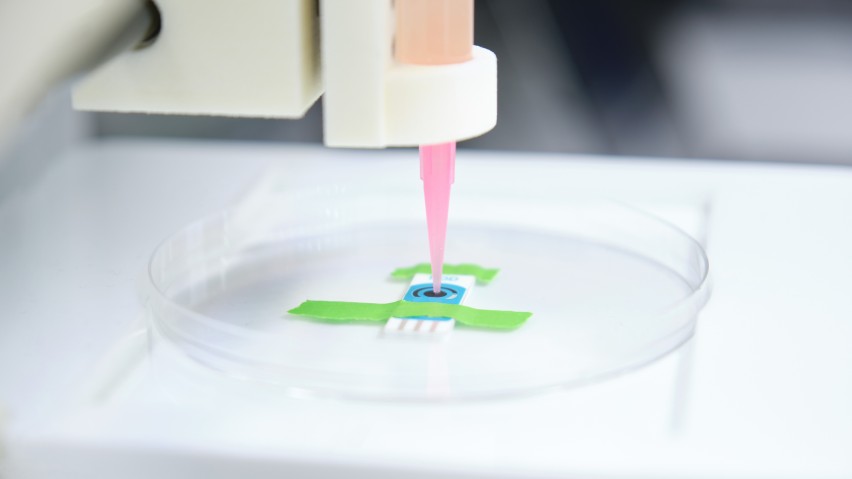
Chang and his team, including Ahmadreza Zaei, first author and doctoral candidate in Chang’s lab, hope to change that by fast-tracking a new 3D printing process that uses microfluidics — the precise manipulation of liquids through tiny channels — to operate at a far smaller scale than has been possible.
Most current 3D bio-printers are extrusion-based, squirting bio-ink out of a nozzle to create structures about 200 microns — around a tenth as wide as a strand of spaghetti. A microfluidics-based printer could print biological objects measuring on the order of tens of micrometers on par with the single cellular scale.
“The scale is very important, because it affects the biology of the organ,” said Chang. “We’re operating at the scale of human cells, and that lets us print structures that mimic the biological features we’re trying to replicate.”
Besides operating on a smaller scale, microfluidics also enables multiple bio-inks, each containing different cells and tissue precursors, to be used interchangeably within a single printed structure, in much the same way that a conventional printer combines colored inks into a single vivid image.
That’s important because while researchers have already created simple organs such as bladders by encouraging the tissue to grow on 3D-printed scaffolding, more complex organs such as livers and kidneys require many different cell types to be precisely combined. “Being able to operate at this scale, while precisely mixing bio-inks, makes it possible for us to reproduce any tissue type,” said Chang.
Scaling down 3D bio-printing requires painstaking research to figure out exactly how different process parameters such as channel structures, flow speed, and fluid dynamics affect the geometries and material properties of printed biological structures. To streamline that process, Chang’s team created a computational model of a microfluidic printing head, enabling them to tweak settings and forecast outcomes without the need for laborious real-world experimentation.
“Our computational model advances a formulaic extraction that can be used to predict the various geometrical parameters of the fabricated structures extruded from the microfluidic channels,” said Zaeri.
The team’s computational models accurately predicted the results of real-world microfluidic experiments, and Chang is using his model to guide experiments on the ways that biological structures with varies geometries can be printed. The results of this research work can be used in the printing of combined multiple cell-types bio-ink that can replicate the tissue with gradients geometrical and compositional properties found at the intersection of bone and muscle.
Chang is also exploring using microfluidic-enabled 3D printing for the in-situ creation of skin and other tissues, enabling patients to have replacement tissues printed directly into a wound. “This technology is still so new that we don’t know precisely what it will enable,” he said. “But we know it will open the door to creating new structures and important new types of biology.”
– Stevens –
About Stevens Institute of Technology Stevens Institute of Technology is a premier, private research university situated in Hoboken, New Jersey. Since our founding in 1870, technological innovation has been the hallmark of Stevens’ education and research. Within the university’s three schools and one college, 8,000 undergraduate and graduate students collaborate closely with faculty in an interdisciplinary, student-centric, entrepreneurial environment. Academic and research programs spanning business, computing, engineering, the arts and other disciplines actively advance the frontiers of science and leverage technology to confront our most pressing global challenges. The university continues to be consistently ranked among the nation’s leaders in career services, post-graduation salaries of alumni, and return on tuition investment.
Stevens media contacts:
Thania Benios
Director of Public Relations
Robin Deehan
Media Relations Manager


