The study, carried out by the team from Universities of Manchester, Cardiff, London and Nijmegen, and Manchester Foundation NHS Trust is published in Nature Communications.
The major funder was the Medical Research Council and the study
The protein, called FHR4, was found by the team to be present at higher levels in the blood of patients with AMD compared to individuals of a similar age without the disease.
The findings were confirmed in 484 patient and 522 control samples from two independent collections across Europe.
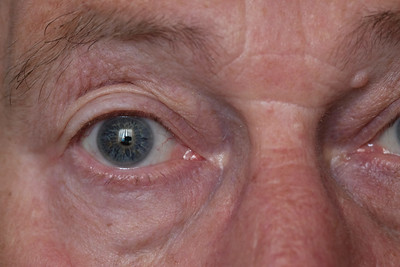
Analyses of eyes donated for research after life also revealed the FHR4 protein was present in the AMD-affected parts of the eye
FHR4 was shown by the team to activate part of the immune system -called the complement system; over activation is a major causal factor of AMD.
FHR4 is one of a group of proteins that regulate the complement system and the genes encoding these proteins are tightly clustered on chromosome 1, the largest human chromosome.
When the team investigated a set of genetic variants across the human genome, they found that genetic variants in this region on chromosome 1 determined the levels of FHR4 in the blood. And they found that the same genetic variants were associated with AMD.
Professor Paul Bishop and Professor Simon Clark, from the University of Manchester were part of the leadership team on the study.
Apart from improving understanding of how AMD is caused, this work provides a way of predicting risk of the disease by simply measuring blood levels of FHR4
 Professor Paul Bishop
Professor Paul BishopProfessor Bishop, who is also a Consultant Ophthalmologist at Manchester Royal Eye Hospital, said: “The combined protein and genetic findings provide compelling evidence that FHR4 is a critical controller of that part of the immune system which affects the eyes.
“We have shown that genetically determined higher blood FHR4 levels leads to more FHR4 in the eye which in turn increases the risk of the uncontrolled immune system response that drives the disease.
“So apart from improving understanding of how AMD is caused, this work provides a way of predicting risk of the disease by simply measuring blood levels of FHR4.
He added: “It also provides a new route to treatment by reducing the blood levels of FHR4 to restore immune system function in the eyes.
“Because treatments options for AMD are limited, this comprehensive understanding of the biology of AMD is a huge boost for scientists finding answers to a problem which causes untold misery for thousands of people in the UK alone.”
Professor Simon Clark, a specialist in the regulation of the complement system in health and disease said: “This study really is a step-change in our understanding of how complement activation drives this major blinding disease.
“Up until now, the role played by FHR proteins in disease has only ever been inferred. But now we show a direct link and, more excitingly, become a tangible step closer to identifying a group of potential therapeutic targets to treat this debilitating disease.”
"Increased circulating levels of Factor H Related Protein 4 are strongly associated with age-related macular degeneration" is published in Nature Communications
Photo: Keith Williamson
manchester.ac.uk

